Reading through the hundreds of stories from healthcare professionals and patients that we receive each year at Costs of Care, it’s apparent there is still a ton of waste in healthcare. I read about physicians struggling to decide whether or not to order an MRI for fear of being sued by a patient if something in the diagnosis is overlooked. I read about patients who don’t have the funds to pay for life saving treatments because of how much they cost.
These stories can be disheartening, but we need to hear them so we can get a handle on the scope of the problem. At Costs of Care, we’re focused on reducing waste and costly treatment in healthcare, addressing the waste problem at the root. We aim to address the issue of costly care by integrating cost decision making at the point of care and provide clinical teams with educational tools to do it effectively. Addressing costs when the patient is in the exam room happens to be the most impactful place to apply lean principles; however, it is one of the least addressed by healthcare organizations today.
If you haven’t noticed, our health system is extremely complex. There are hundreds of surgical and non-surgical sub-specialties, thousands of hospital systems, and billions of medications prescribed each year. Physicians have more treatment options than even just a few years ago and patients today have an overwhelming amount of care information available; yet, we struggle to provide holistic, coordinated care. As a patient, you can now get various hospital quality data online, compare a hospital to those in other cities, and rate a physician on both quality as well as bedside manner. There are literally thousands of locations to get a hip replacement and just as many options on who you want to perform it. It is no wonder that patients are feeling confused and looking to find value in healthcare.
Today, front line clinicians are being asked to provide even more cost-efficient care to patients yet few understand how to do so. There is a new focus on efficiency in treatment options and today’s patients are more cost savvy than their predecessors. We must ensure value while reducing costs and improving quality outcomes.
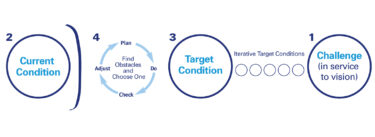
To assist organizations and individual clinicians with providing more cost-conscious care, we have developed a clear framework to address overtreatment and non-value added treatment. The “COST” framework outlines 4 key areas of focus:
- Culture – organizations must value cost-consciousness and resource stewardship
- Oversight – there must be clear accountability for cost-conscious decision making
- Systems Change – systems should guide cost-conscious decisions and be supported by policy
- Training – information sharing needs to exist to increase the skills and knowledge of clinicians
The main objective of the framework is to drive cost-conscious decision making, but the framework itself is not sufficient in reducing costs. Individual practitioners and organizations must instill the framework daily in order to see results. However, this framework, aligned with lean principles, also reminds us to identify value and focus on identifying areas of waste in the current system.
Applying the Framework
At my hospital, we have a dedicated department that works to improve organizational processes and partners with physicians to test theories on ways to reduce waste. We have interdisciplinary teams of clinicians and administrators from the front lines working together to change the way we provide care. This is something that has been ingrained in our culture. All levels of management and clinical staff are involved with transforming the organization and there is clear support/oversight from senior leadership to empower teams to create change and help us succeed.
Our progress has been remarkable though not yet complete. We’re also currently working to install a new electronic medical record system and have designed future workflows to enable these changes. Finally, this past year, we have asked our teams to spend a lot of time on this initiative and it has pulled them away from their daily responsibilities. However, we’re currently engaging our teams to align a comprehensive training program that both encompass our newly designed workflows along with system changes. Only by applying all areas of the “COST” framework will we be truly successful in impacting value at the hospital.
As the healthcare industry continues to transform and progress towards providing more value-based care while improving outcomes, patients should always be the focus. I encourage others to focus on value. And not only look to lean methodology for solving our industry’s issues, but to experiment with the “COST” framework. Identifying waste will continue to improve and develop a strong organizational culture, develop stronger leadership oversight, and enable systems change. In our work, we’ve seen transformation finally come to healthcare. Through the “COST” framework, we are shaping the way value is defined with patients.