The late and widely respected Princeton health economist Uwe Reinhardt famously answered the question, “why does U.S. healthcare cost so much?” with the observation, “It’s the prices, stupid.”
Now there’s more evidence that Prof. Reinhardt was right: a recent article (paywalled) in the prestigious Journal of the American Medical Association(JAMA) by Irene Papanicolas, Liana Woskie, and Ashish Jha reviews key data about healthcare in the U.S. and other high-income countries and finds that while Americans use more high-end imaging (MRI and CT) than other countries, in general, the utilization of medical services – rates of hospitalization, in particular – are pretty comparable between the U.S. and other countries.
So what’s the difference? The cost of individual components of the national healthcare bill are all significantly more expensive here than elsewhere: hospital charges, physician compensation (and therefore prices), pharmaceuticals – all much, much higher in the U.S.
The article also notes that administrative costs – those expenses related to “planning, regulating and managing health systems and services” – are 8% of the (much higher) U.S. healthcare cost structure, instead of the 1-3% found abroad. As a “recovering healthcare bureaucrat,” I used to be the recipient of a portion of that bloated 8%! But the higher admin costs here also don’t much surprise me: the U.S. has the most privatized healthcare system of any of these countries, with a plethora of private (and governmental) insurers paying claims to tens of thousands of hospitals and health systems and millions of individually licensed physicians, with huge variations in pricing, care-delivery processes, and almost no standardization in billing procedures.
OK – so U.S. prices are higher, and since “somebody’s costs are somebody else’s income,” lowering prices means inflicting pain on the stakeholders in the healthcare system. We also know that the local hospital is the biggest, or nearly the biggest, employer in most U.S. Congressional districts, so the politics of squeezing dollars out of the healthcare system will be fierce. Should the rest of us care? Well, since the healthcare system is $3 trillion a year or almost 18% of the U.S. economy, if healthcare gets squeezed, the rest of us will surely feel the pinch, either in reduced services or impact to local employment.
Now, not every observer would agree that prices are the culprit. The health journalist Shannon Brownlee is the author of Overtreated: Why Too Much Medicine is Making Us Sicker and Poorer, and you can guess from the title that it’s her belief that we use too much of everything in American medicine: tests, drugs, hospitalizations, fancy technology – and not enough public health, wellness, and prevention.
Barbara Ehrenreich, who wrote about the plight of the low-wage worker in the U.S. in Nickel and Dimed, has a new book out called Natural Causes: An Epidemic of Wellness, the Certainty of Dying, and Killing Ourselves to Live Longer. In it, she reveals that at age 75, she’s decided to forego additional medical checkups, screenings, testing, and try to accept the fact and outcome of the natural aging process. Not for everyone, perhaps, but along the way she makes some telling observations about the costs and harm inflicted by the healthcare system in our search for life eternal.
“OK, former healthcare guy,” you ask. “Important issue, but what’s it have to do with lean thinking and practice?” More to the point: how can we bring lean thinking and practice to solve the huge problem of high U.S healthcare cost and low performance?
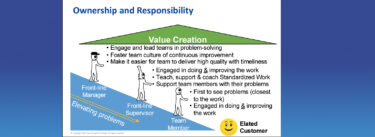
Well, of course, we are working on it, although our efforts are modest in relation to the enormous scale of the system. We have several healthcare partners at LEI, including the Lynn Community Health Center and their dynamic new CEO, Dr. Kiame Mahaniah, who presented at our recent Nashville Lean Transformation Summit. Our colleagues at Catalysis bring lean thinking and practice to the healthcare space exclusively; their Lean Healthcare Transformation Summit is upcoming in June, and you can read Dr. John Toussaint’s excellent article for the Harvard Business Review, “Why Process Is U.S. Healthcare’s Biggest Problem” about bringing the tools of TPS and design thinking to bear on redesigning healthcare workflow.
At the hospital where my LEI colleague Alice Lee and I both worked, we sponsored a big initiative on “nursing documentation,” designed to reduce the mountain of forms that each floor nurse needed to complete each day for every patient to something more reasonable. It took a big commitment – a couple of dozen nurses pulled off the floor, their roles backfilled by other staff, for a day a week for several months – to understand the workflow and map the value stream. But the result was a dramatic reduction in administrative waste that freed these nurses to spend time where they should be: at the patient bedside.
Change may come from the startup world as well: last week I had the opportunity to speak to a group of young entrepreneurs, mostly physicians and researchers, at the Yale Medical School “Innovation to Impact” program that aims to accelerate innovation in the behavioral health area. We are seeing the impact of “telehealth” and smartphone technology to take the place of office visits for many simple medical needs and screening. Is there really a need to schedule a routine review by a dermatologist when suspicious lesions can be imaged on a smartphone and evaluated by a licensed specialist a world away? There is a world of innovation swirling around healthcare, looking to exploit the obvious failure of the current system to create sufficient value for the patient.
So while lean thinking and practice can show the way to better value creation in healthcare, I believe that lean thinkers also have to insist that the current state of the system runs roughshod over “respect for people.” When increases in healthcare costs eat up wage gains, when Amazon – that darling of Wall Street and the tech world – is also a major employer of workers who rely on government SNAP payments to feed their families– something is very, very wrong. We need to both improve the work in healthcare to remove waste and create value and be advocates for enough “social heijunka” to ensure that resources going to that sector don’t impoverish frontline workers across our society.
In the months ahead, I’ll use this space to keep you informed about these issues and the improvements being made by our healthcare partners. In the meantime, use the “comments” to tell me what you think.